Reading time
12 min read
Future of Ophthalmology: 2025 Top Trends
In a recent survey conducted by our team, we asked eye care specialists to identify the most transformative trends in ophthalmology by 2025. The results highlighted several key areas, with artificial intelligence (AI) emerging as the clear frontrunner, cited by 78% of respondents.
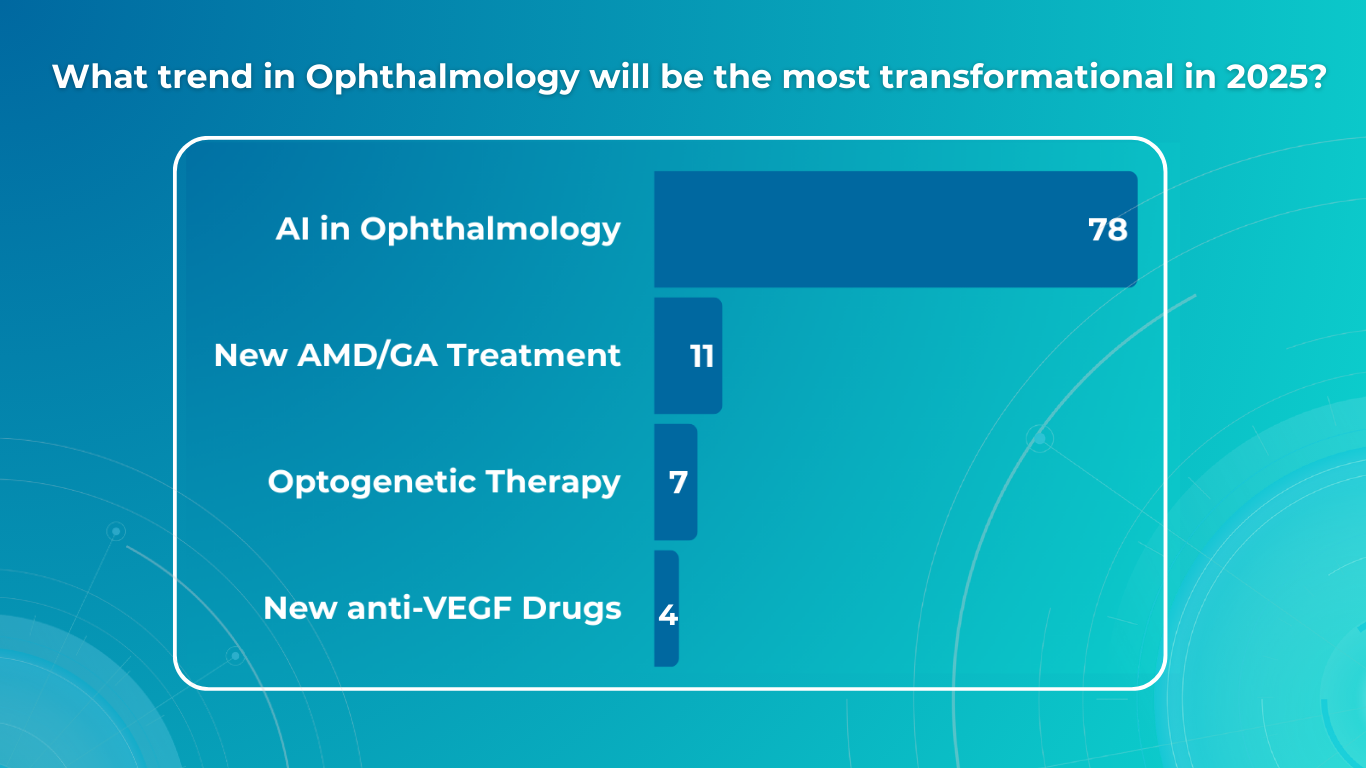
However, the survey also underscored the significant impact of optogenetics, novel AMD/GA therapies, and the continuing evolution of anti-VEGF treatments. This article will explore the practical implications of these advancements, providing an overview of how they are poised to reshape diagnosis, treatment, research, and, ultimately, patient outcomes in ophthalmology.
FDA-cleared AI for OCT analysis
Building upon the survey’s findings, we begin with the most prevalent trend:
AI in Ophthalmology

AI in Clinical Eye Care Practice
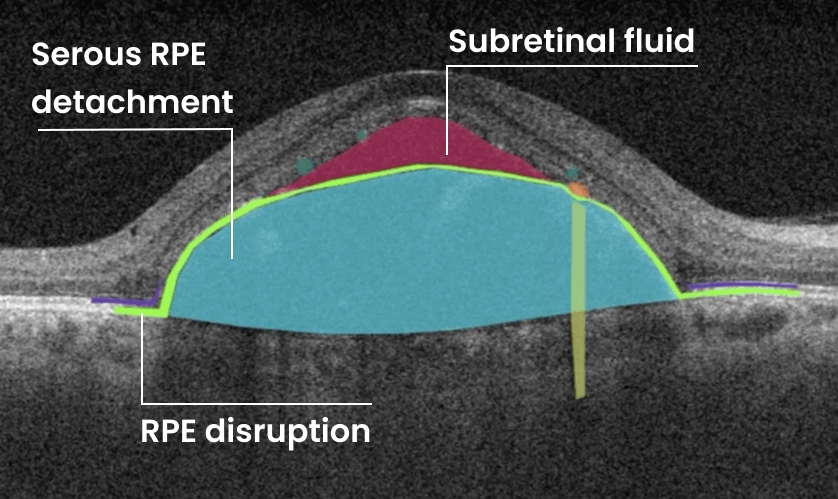
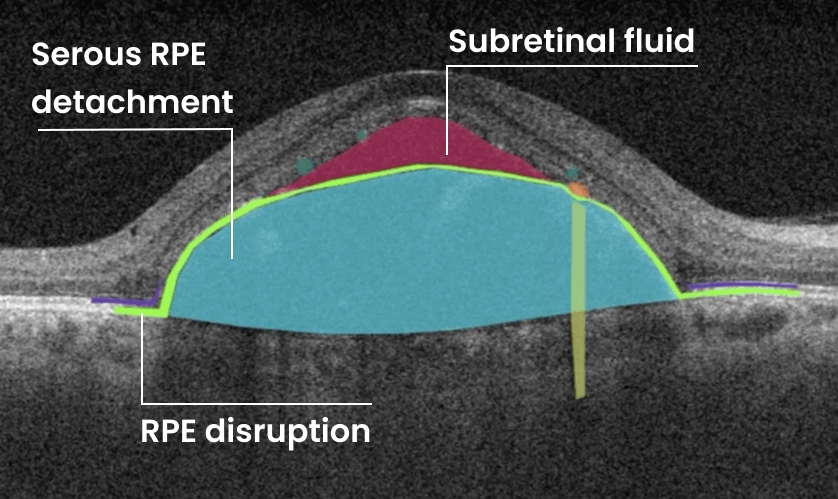
With the increasing prevalence of conditions like diabetic retinopathy and age-related macular degeneration, there is a growing need for efficient and accurate screening tools. And AI is already valuable for eye-care screening: algorithms can analyze retinal images and OCT scans to identify signs of these diseases, enabling early detection and timely intervention.

AI-powered screening tools can also help identify rare inherited retinal dystrophies, such as Vitelliform dystrophy and Macular telangiectasia type 2. These conditions can be challenging to diagnose, but AI algorithms can analyze retinal images to detect subtle signs that human observers may miss.
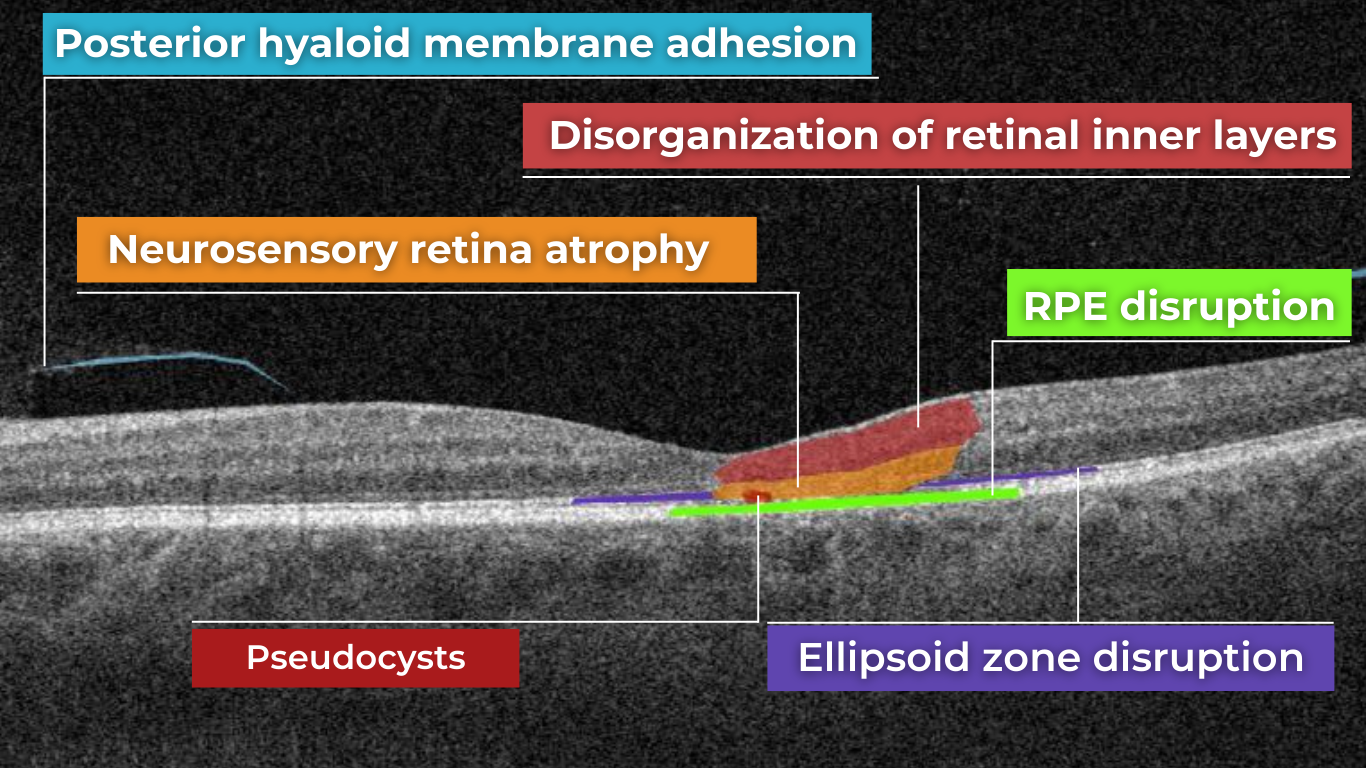
Biomarkers of MacTel 2 detected and visualized by AI for OCT platform, Altris AI
AI also starts to play a crucial role in glaucoma management. Early detection of glaucoma demands exceptional precision, as the early signs are often subtle and difficult to detect. Another significant challenge in glaucoma screening is the high rate of false positive referrals, which can lead to unnecessary appointments in secondary care and cause anxiety for patients—yet delayed or missed detection of glaucoma results in irreversible vision loss for millions of people worldwide. So, automated AI-powered glaucoma analysis can offer transformative potential to improve patient outcomes.
One example of promising AI technology is Altris AI, artificial intelligence for OCT scan analysis, which has introduced its Advanced Optic Disc (OD) Analysis that provides a comprehensive picture of the optic disc’s structural damage, allowing detailed glaucoma assessment for treatment choice and monitoring.
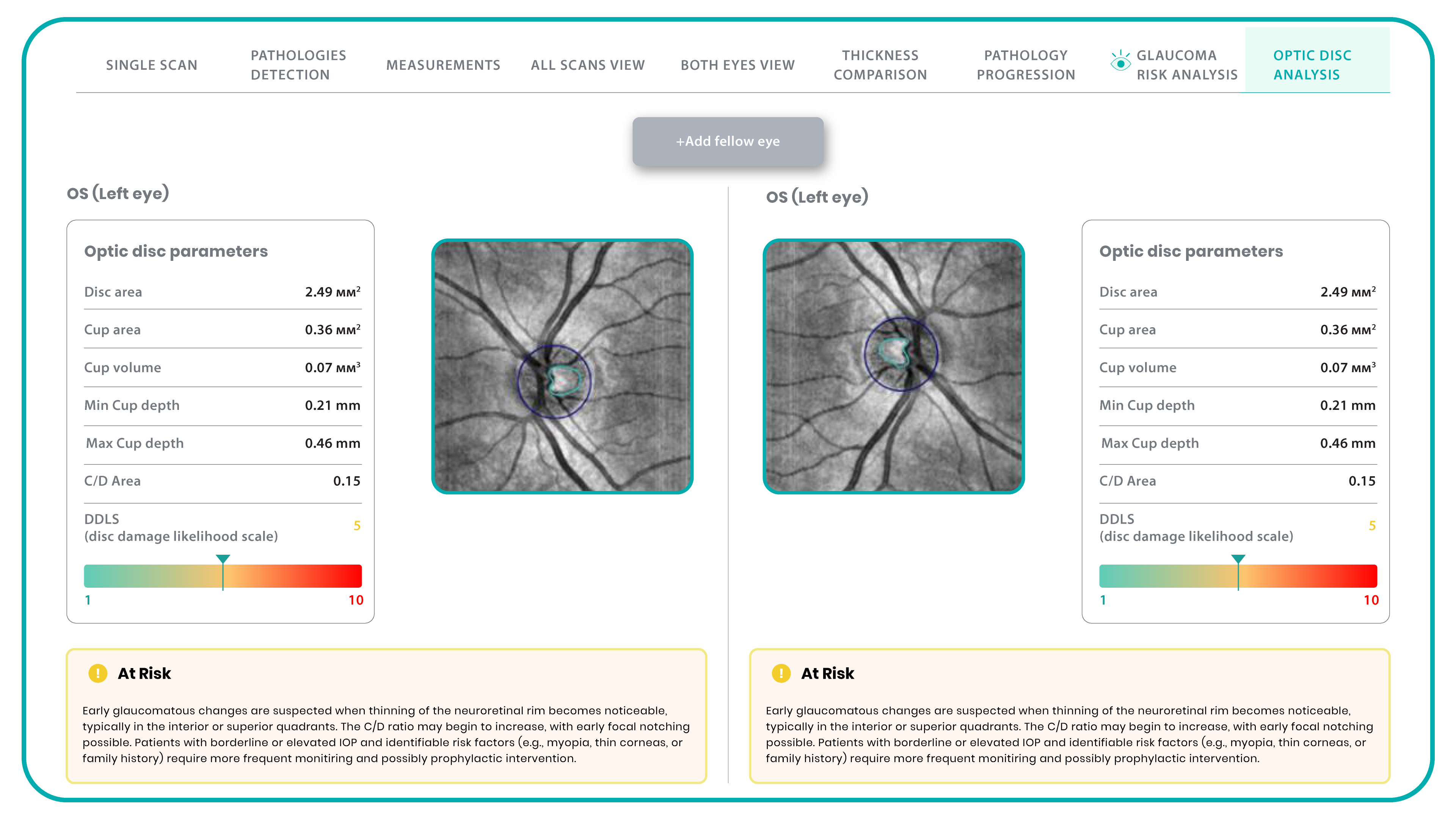
This OD module evaluates optic disc parameters using OCT, providing personalized assessments by accounting for individual disc sizes and angle of rim absence. Such a tailored approach eliminates reliance on normative databases, making evaluations more accurate and patient-specific.
Furthermore, it enables cross-evaluation across different OCT systems, allowing practitioners to analyze macula and optic disc pathology, even when data originates from multiple OCT devices. Key parameters evaluated by Altris AI’s Optic Disc Analysis include disc area, cup area, cup volume, minimal and maximum cup depth, cup/disc area ratio, rim absence angle, and disc damage likelihood scale (DDLS).

AI for Clinical Trials and Research
AI is revolutionizing clinical trials and research in ophthalmology. One such key application of AI is biomarker discovery and analysis. Algorithms can analyze large datasets of medical images, such as OCT scans, to identify and quantify biomarkers for various eye diseases. These biomarkers can be used to assess disease progression, monitor treatment response, and predict clinical outcomes.
AI is also being used to improve the efficiency and effectiveness of clinical trials. By automating the process of identifying eligible patients for clinical trials, AI can help researchers recruit participants more quickly and ensure that trials include appropriate patient populations, accelerating the development of new treatments.
Algorithms can analyze real-world data (RWD) collected from electronic health records and other sources to generate real-world evidence (RWE). RWE provides valuable insights into disease progression, treatment patterns, and long-term outcomes in everyday clinical settings, complementing the findings of traditional randomized controlled trials.
Oculomics
Integrating digitized big data and computational power in multimodal imaging techniques has presented a unique opportunity to characterize macroscopic and microscopic ophthalmic features associated with health and disease, a field known as oculomics. To date, early detection of dementia and prognostic evaluation of cerebrovascular disease based on oculomics has been realized. Exploiting ophthalmic imaging in this way provides insights beyond traditional ocular observations.
For example, the NeurEYE research program, led by the University of Edinburgh, is using AI to analyze millions of anonymized eye scans to identify biomarkers for Alzheimer’s disease and other neurodegenerative conditions. This research can potentially revolutionize early detection and intervention for these devastating diseases.
Another effort spearheaded by researchers from Penn Medicine, Penn Engineering is exploring the use of AI to analyze retinal images for biomarkers indicative of cardiovascular risk. AI systems are being trained on fundus photography to detect crucial indicators, such as elevated HbA1c levels, a hallmark of high blood sugar, and a significant risk factor for both diabetes and cardiovascular diseases.

AI analysis of retinal characteristics, such as retinal thinning, vascularity reduction, corneal nerve fiber damage, and eye movement, has shown promise in predicting Neurodegenerative diseases. Specifically, decreases in retinal vascular fractal dimension and vascular density have been identified as potential biomarkers for early cognitive impairment, while reductions in the retinal arteriole-to-venular ratio correlate with later stages.
Moving from AI, we now turn to another significant trend identified in our survey:
Optogenetics
Optogenetics represents a significant leap forward in ophthalmic therapeutics, offering a potential solution for vision restoration in patients with advanced retinal degenerative diseases, where traditional gene therapy often falls short. While gene replacement therapies are constrained by the need for viable target cells and the complexity of multi-gene disorders like retinitis pigmentosa (RP), optogenetics offers a broader approach.

This technique aims to circumvent the loss of photoreceptors by introducing light-sensitive proteins, known as opsins, into the surviving inner retinal cells and optic nerve, restoring visual function through light modulation. This method is particularly advantageous as it is agnostic to the specific genetic cause of retinal degeneration.
By delivering opsin genes to retinal neurons, the technology enables the precise manipulation of cellular activity, essentially transforming these cells into new light-sensing units. This approach can bypass the damaged photoreceptor layer, transmitting visual signals directly to the brain.
Several companies are pioneering advancements in this field. RhyGaze, for example, has secured substantial funding to accelerate the development of its lead clinical candidate, a novel gene therapy designed for optogenetic vision restoration. Their efforts encompass preclinical testing, including pharmacology and toxicology studies, an observational study to define clinical endpoints, and a first-in-human trial to assess safety and efficacy. The success of RhyGaze’s research could pave the way for widespread clinical applications, significantly impacting the treatment of blindness globally.

Nanoscope Therapeutics is also making significant strides with its MCO-010 therapy. This investigational treatment, administered through a single intravitreal injection, delivers the Multi-Characteristic Opsin (MCO) gene, enabling remaining retinal cells to function as new light-sensing cells. Unlike earlier optogenetic therapies that required bulky external devices, MCO-010 eliminates the need for high-tech goggles, simplifying the treatment process and enhancing patient convenience. The ability to restore light sensitivity without external devices represents a major advancement, potentially broadening the applicability of optogenetics to a wider patient population.

Another critical area of innovation highlighted in our survey is the advancement of treatments for AMD and GA.
New AMD/GA Treatment
Age-related macular degeneration (AMD) and geographic atrophy (GA) represent a significant challenge in ophthalmology, demanding innovative therapeutic strategies beyond the established anti-VEGF paradigm.
Gene Correction
Gene editing is emerging as a powerful tool in the fight against AMD and GA, potentially correcting the underlying genetic errors that contribute to these diseases. Essentially, it allows us to make precise changes to a patient’s DNA.
Traditional gene editing techniques often rely on creating ‘double-strand breaks’ (DSBs) in the DNA at specific target sites, which are like precise cuts in the DNA strand. These cuts are made using specialized enzymes, like CRISPR-Cas9, which act as molecular scissors. While effective, these methods can sometimes introduce unwanted changes at the cut site, such as small insertions or deletions.
After a DSB is made, the cell’s natural repair mechanisms kick in. There are two main pathways:
- Non-Homologous End Joining (NHEJ): This is the cell’s quick-fix method. It essentially glues the broken ends back together. However, this process can sometimes introduce errors, leading to small insertions or deletions that can disrupt the gene’s function.
- Homology-Directed Repair (HDR): This is a more precise repair method. It uses a ‘donor’ DNA template to guide the repair process, ensuring accuracy. However, HDR is more complex and less efficient, especially in non-dividing cells.
To overcome these limitations of traditional gene editing, researchers have developed more precise techniques:
- Base Editing: This technique allows scientists to change a single ‘letter’ in the DNA code without creating DSBs.
- Prime Editing: This advanced technique builds upon CRISPR-Cas9, allowing for a wider range of precise DNA changes. It can correct most disease-causing mutations with enhanced safety and accuracy.
- CASTs (CRISPR-associated transposases): This method enables larger DNA modifications without creating DSBs, offering a safer approach to genetic correction.
Why does this matter for AMD and GA? These advancements in gene editing are crucial for addressing the genetic roots of these pathologies. We can potentially develop more effective and targeted therapies by precisely correcting the faulty genes that contribute to these diseases. The technologies are still being researched, but they hold great promise for the future of ophthalmology.
Cell Reprogramming
Cell reprogramming offers a novel approach to regenerative medicine, with the potential to replace damaged retinal cells. This technique involves changing a cell’s fate, either in vitro or in vivo. In vitro reprogramming involves extracting cells, reprogramming them in a laboratory, and then transplanting them back into the patient. In vivo reprogramming, which directly reprograms cells within the body, holds particular promise for retinal diseases. This approach has succeeded in preclinical studies, demonstrating the potential to restore vision in conditions like congenital blindness.
Vectors and Delivery Methods
The success of gene therapy relies on efficiently delivering therapeutic genes to target retinal cells. Vectors are essentially delivery vehicles, designed to carry therapeutic genes into cells. These vectors can be broadly classified into two categories: viral and non-viral. Vectors, both viral and non-viral, are crucial for this process.
Viral vectors are modified viruses that have been engineered to remove their harmful components and replace them with therapeutic genes. They are highly efficient at delivering genes into cells, as they have evolved to do just that. Adeno-associated viruses (AAVs) are the most commonly used viral vectors in ocular gene therapy due to their safety profile and cell-specificity. The diversity of AAV serotypes allows for tailored gene delivery to specific retinal cell types.
Non-viral vectors, on the other hand, are synthetic systems that don’t rely on viruses. They can be made from lipids, polymers, or even DNA itself. While they may be less efficient than viral vectors, they offer safety and ease of production advantages.
Advances in vector design, whether viral or non-viral, are focused on enhancing gene expression, cell-specificity, and carrying capacity.
Now, let’s examine the ongoing evolution of anti-VEGF treatments, a cornerstone of modern retinal care.
New Anti-VEGF drugs
The landscape of ophthalmology has undergone a dramatic transformation since the early 1970s when Judah Folkman first proposed the concept of tumor angiogenesis. His idea sparked research that ultimately led to the identification of vascular endothelial growth factor (VEGF) in 1989 and the development of anti-VEGF therapies, revolutionizing the treatment of neovascular eye diseases, dramatically improving outcomes for patients with wet AMD, diabetic retinopathy, and retinal vein occlusions.
Population-based studies have shown a substantial reduction (up to 47%) in blindness due to wet AMD since the introduction of anti-VEGF therapies. However, significant gaps remain despite this progress, especially regarding treatment durability. Anti-VEGF drugs require frequent intravitreal injections, which can be difficult for patients due to time commitments, financial costs, and potential discomfort. Although newer agents have extended treatment intervals, patient adherence and undertreatment challenges persist in real-world settings. Innovative approaches are being investigated to address these unmet needs to increase drug durability and reduce the treatment burden.
Tyrosine Kinase Inhibitors
One approach to increasing treatment durability is using tyrosine kinase inhibitors (TKIs). TKIs are small-molecule drugs that act as pan-VEGF blockers by binding directly to VEGF receptor sites inside cells, offering a different action mechanism than traditional anti-VEGF drugs that target circulating VEGF proteins.
Currently, TKIs are being investigated as maintenance therapy, primarily in conjunction with sustained-release delivery systems. Two promising TKIs for retinal diseases are axitinib and vorolanib. In a bioresorbable hydrogel implant, Axitinib is being studied for neovascular AMD and diabetic retinopathy. Vorolanib, in a sustained-release delivery system, is also being investigated for neovascular AMD. These TKIs offer the potential for less frequent dosing, reducing the treatment burden for patients.
Port Delivery System
The Port Delivery System (PDS) is a surgically implanted, refillable device that provides continuous ranibizumab delivery for up to 6 months. While it’s FDA-approved for neovascular AMD, it’s also being investigated for other retinal diseases, such as diabetic macular edema and diabetic retinopathy.
Although the PDS faced a voluntary recall due to issues with septum dislodgment, it has returned to the market with modifications. The PDS offers the potential for significantly reduced treatment frequency for a subset of patients. However, challenges remain, including the need for meticulous surgical implantation and the risk of endophthalmitis.
Nanotechnology
Nanotechnology offers promising solutions to overcome limitations of current ocular drug delivery. The unique structure of the eye, with its various barriers, poses challenges for drug delivery. Topical administration often fails to achieve therapeutic concentrations, while frequent intravitreal injections carry risks. Nanotechnology can improve drug solubility, permeation, and bioavailability through nanoparticles, potentially extending drug residence time and reducing the need for frequent injections. Several nanoparticle systems, lipid and polymeric, are being studied for ocular drug delivery, offering hope for more effective and less invasive treatments.
FDA-cleared AI for OCT analysis
Summing up
The advancements discussed in this article, encompassing AI, optogenetics, novel AMD/GA therapies, and refined anti-VEGF treatments, collectively signal a transformative era for ophthalmology. As highlighted by the survey results, AI probably encompasses most of the changes by redefining diagnostic and clinical workflows through its capacity for image analysis, biomarker identification, and personalized patient management.
Optogenetics offers a distinct pathway to vision restoration, bypassing limitations of traditional gene therapy. The progress in AMD/GA treatments, particularly gene editing and cell reprogramming, presents opportunities for targeted interventions. Finally, the evolution of anti-VEGF therapies, with innovations in drug delivery and sustained-release mechanisms, addresses persistent challenges in managing neovascular diseases.
These developments, driven by technological innovation and clinical research, promise to enhance patient outcomes and reshape the future of ophthalmic care.